WHAT IS THE PROSTATE?
The first step toward understanding how the prostate affects your health is to learn what the prostate is and how it functions.
It is surprising how little many men know about such an important part of their anatomy.
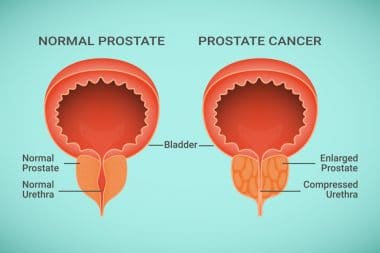
The prostate is an important segment of the male reproductive system. It is a gland that is located in the lower abdominal cavity, just below the bladder, in front of the rectum and behind the pubic bone. It partially surrounds the urethra. The urethra is the channel that carries urine to the penis from the bladder and it runs right through the prostate.
A healthy prostate is about the size of a walnut, weighs approximately 1 ounce and is shaped similar to a donut.
There are “seminal vesicles” that are attached to the prostate. They produce a protein that mixes with prostatic fluid which forms semen. How this works is that tubes from the testicles carry sperm up to the prostate where sperm is mixed with the seminal vesicle and prostatic fluids.
This fluid is ejaculated during orgasm through ejaculatory ducts that connect to the urethra. In addition, the prostate helps to control the flow of urine.
Nearly every man will experience some type of prostate problem during his lifetime. Men who are over forty-five may experience an enlargement of the prostate. While this is not a problem in itself, it is uncomfortable and can be a forerunner to other more serious maladies which we will discuss further.
The prostate actually continues to grow throughout life, but grows very slowly after the age of twenty-five. Enlargement of the prostate is part of the normal aging process due to hormonal changes and usually does not become a serious problem until a man reaches sixty years of age.
SYMPTOMS OF PROSTATE PROBLEMS
Enlargement of the prostate is called benign prostate hypertrophy, or BPH. While this growth is usually considered a nuisance, if a man experiences problems with burning, or difficult urination at any time, the prudent course of action is consulting a urologist.
Other symptoms may be:
· A feeling of having to push out urine
· A sensation that the bladder is not emptying
· Increased urinating, especially at night
· Intermittent starting and stopping of the urinary stream
After a diagnosis of BPH, many men will just continue to live with the symptoms and subsequent discomfort. It is not a life threatening condition, and there are treatments. In some cases surgery might be considered if the enlargement is significant.
Ignoring BPH can be extremely dangerous and lead to other disease such as kidney infections or damage as the urine can back up into the kidneys because of the blockage of an enlarged prostate. There can also be an occurrence of bladder infections.
There is a huge difference between BPH and prostate cancer. BPH is a normal part of aging. Prostate cancer is a condition where prostate cells grow exponentially and out of control. These cells create tumors that may spread to any part of the body.
Numerous health organizations report that 1 in 6 men will experience prostate cancer. However, if the condition is diagnosed early, approximately 99.3% of them will survive. The key is early detection.
DIAGNOSTIC TESTING
Prostate cancer can occur in any man, but there are certain “risk groups.” Younger African American men appear to have twice the risk and fatalities of Caucasians. Sadly, many are diagnosed before they reach the age of 50.
Another risk group is men who have a family history of prostate cancer, placing them in the same group who may contract the disease before the age of 50.
The only method to determine whether you are at risk for prostate cancer is diagnostic testing. The earlier you are screened the higher your chances of survival. Let”s explore some of the diagnostic options.
Digital Rectal Exam (DRE)
Testing begins with a digital rectal exam (DRE). This examination has been the benchmark for discovering cancer as well as BPH. Your doctor can determine the condition and size of the prostate by inserting a gloved finger into the rectum.
Prostate Specific Antigen (PSA)In the mid-1980s’ the FDA approved the use of monitoring blood levels for prostate specific antigen (PSA). At that time, this was considered a major breakthrough in the diagnosis and treatment for prostate cancer.
Here”s why. PSA readings specifically target prostate cells. A healthy prostate gland produces a constant level, usually 4 nanograms per milliliter which is considered as a PSA reading of “4” or less.
Cancer cells produce growing amounts that escalate. They correlate with the severity of cancer. A PSA level greater than 4 will give the doctor some cause for investigation. If the level reaches 10 he will have cause to consider the presence of prostate cancer. An amount over 50 may indicate that the cancer has spread to other parts of the body.
A PSA test usually measures the total amount that is attached to blood proteins. However, later research gained an FDA approval for a test called the Tandem R test. This test also gives a measure of the total PSA and reads another component called free PSA. Free PSA floats unbound in blood.
Have these two tests to compare helps to rule out prostate cancer in men whose PSA is just mildly elevated due to other causes. A 1995 study in the Journal of the American Medical Association shows that a free PSA test reduces unnecessary prostate biopsies by 20% in certain patients whose PSA is between 4 and 10.
As newer sophisticated methods are made available, it is creating a controversy among the healthcare community regarding “when” men should be screened, how often and whether to screen men under 50 with no symptoms.
Some are saying that mass screening is expensive while others point out reductions in mortality rates when early screening diagnoses prostate cancer. The jury is still somewhat “out” on that debate, but it never hurts to err on the side of caution. It is your body, after all!
It should be noted that both The American Urological Association and The American Cancer Society recommend annual PSA test for all men over 50 and for those at high risk over 40.
Take the case of Joe. A healthy, 36 year old, robust father of two was required to take a routine physical exam for his work-related insurance. During this exam, his doctor noted that his prostate was enlarged. Unfortunately, the resulting tests proved that he did indeed have prostate cancer. Further investigation revealed that he was “at risk” based on family history.
Why take chances? Get yourself screened so you have a benchmark, then having annual screening. Remember, prostate cancer is slow growing so the odds are in your favor when detected early.
Urine Test
A standard urine test can also help to diagnose prostate problems by screening for blood or infection. The chemical tests will also check for liver, diabetes or kidney disease.
Hyperplasia INTRAVENOUSPYELOGRAM (IVP)
This test is actually an X-ray. Dye is injected into one of the major veins. While the dye is circulating, pictures of vital organs are taken. This test will record the progress of the dye through the kidneys, bladder and ureter tubes (the tubes that drain the kidneys). This test is more or less optional since most men who have enlargement of the prostate usually have no abnormalities of the ureter tubes or kidneys in a normal urinalysis.
Bladder Ultrasound
This is a simple procedure that can be conducted right in the doctors’ office. It is non-invasive and determines if there is urine left in the bladder after urination. If a large amount of urine remains, it could be an indicator of enlarged prostate that is not allowing the bladder to be completely emptied.
Prostate Ultrasound
This is a test to estimate the size of the prostate by using state of the art software that helps guide the physician. The prostate ultrasound is also important if a biopsy is called for which we will discuss later.
Uroflow
This is a simple test that entails the patient urinating into a container and measuring how strong the stream of urine is.
Radionuclide Bone Scan
A test that can be used if staging (see below) indicates that cancer has spread into the lymph nodes. If the tumor has spread to the lymph nodes, bone commonly follows. However, if PSA levels are under 10ng and there is no indication of bone pain, physicians find that the presence is so unlikely that this procedure is skipped.
Cystoscopy
This test allows the physician to visually examine the bladder and prostate. This is done by inserting an instrument through the urethra.
Computed Axial Tomography (CAT)
This is another test that could identify cancer in remote areas of the body. Without probable cause, like the Radionuclide Bone Scan above, it is probably unnecessary just as the
Magnetic Resonance Imaging (MRI)
This test may be unnecessary, especially if the prostate cancer is localized.
Pelvic Lymph Node Dissection
Considered to be the “final check” to determine if cancer has spread, this procedure can be completed through normal open surgery but more often is conducted using a fiber optic probe that is inserted through a small incision in your abdomen.
All of these diagnostic tests are tools to determine whether there is a possibility of cancer present in the prostate and if so, just how invasive it may be.
However, there is only one way certain method to determine the presence of cancer cells and that is by examining the tissue itself.
Based on the findings of the tests we have discussed, if a physician determines that there may be cancer cells he will recommend a biopsy.
A biopsy is conducted by a urologist and the procedure is normally done right in his office. Here is where the ultrasound we discussed previously comes into play. Using a transrectal ultrasound (TRUS), the doctor will image the prostate by using sound waves by inserting an instrument into your rectum. This allows the doctor to “image” the prostate. He will use biopsy needles that are hollow into any area of the prostate that looks or feels suspicious. Small bits of tissue are extracted through the needle. You may feel a stinging sensation.
Depending on the reasons for the biopsy, the doctor may take samples randomly. For instance, if the biopsy is conducted due to elevated PSA instead of a suspected abnormality in the prostate gland, as many as a half dozen or more samples may be taken. This is considered a “pattern biopsy” and is done to help determine the size and invasiveness of any cancer. Even though you may have multiple samples, a biopsy can still miss some cancers.
Once the biopsy is complete, the tissue samples are taken to a pathologist to determine the presence of cancer cells.
Normal prostate cells are usually uniform in size and are neatly patterned when viewed under a microscope. They appear similar to one another in an orderly manner.
Abnormal cells change their appearance and are not well defined. They will usually appear as misshapen and irregular.
As they deteriorate, a tumor can appear. Tumors can be benign (non-cancerous) or malignant (cancerous).
Tumor Grading
If the pathologist determines the presence of prostate cancer, he will “grade” each of the tissue samples. This will determine how advanced beyond normal the cancerous tissue has developed. This grading system gives the physician a good idea as to how the tumor is behaving. Tumors with a low grade are most likely to be slow-growing. Tumors with a high grade are more apt to spread aggressively or may have already spread outside of the prostate. If the latter is true, it is said to be “metastasized.”
The actual grading system most widely used by pathologists is the Gleason Grading System, developed in 1977 by Pathologist Donald Gleason. You will find the Gleason Scores in numerous places on and off the internet as it is a standard method, but we have provided them for you here.
Gleason Scores
The Gleason grading system assigns a grade to each of the two largest areas of cancer in the tissue samples. Grades range from 1 to 5, with 1 being the least aggressive and 5 the most aggressive. Grade 3 tumors, for example, seldom have metastases, but metastases are common with grade 4 or grade 5.
The two grades are then added together to produce a Gleason score. A score of 2 to 4 is considered low grade; 5 through 7, intermediate grade; and 8 through 10, high grade. A tumor with a low Gleason score typically grows slowly enough that it may not pose a significant threat to the patient in his lifetime.
Once the grade is established, your physician will need to have additional information before determining a course of treatment. He will need to “stage” your tumor which is dependent upon the size and how far it has spread.
There are two systems used for “staging” the tumor. One of them is TNM and the other is ABCD Rating. They both evaluate the size of the tumor and the spread in reference to nearby lymph nodes and if the cancer has spread beyond those parameters.
The staging system determines whether the tumor is “Localized,” “Regional” or Metastatic. Within each of these categories are divided into categories that are more precise.
Localized
Using the TNM method, you have Stage I (could also be referred to as T1.) These are tumors that cannot be felt. Using the ABCD method the staging is considered “A.”
TNM Stage II or B or T2 are tumors that you can feel but are still confined to the prostate gland.
Regional
In Stage III or C or T3 tumors have broken through the prostate capsule. They may have invaded the seminal vesicles.
T4 indicates that tumors are growing into muscles and organs that are nearby.
Metastatic
Stage IV, D or N+ or M+. This staging refers to tumors that have invaded either the pelvic lymph nodes (N+) or into other distant areas of the body (M+).
If you receive a diagnosis of cancer and different treatment options from your doctor, it would be prudent to get a second opinion. This is a normal practice and one which can help you make intelligent decisions about the most important step you may take in your life.
Getting that second opinion may confirm the diagnosis but help you to adjust the staging and your treatment options. A second opinion may also lead you to a special clinical trial of new cancer treatments that your current physician is not aware of.
Try and locate a prostate cancer support group in your area. Speaking to other men who have experienced prostate disease can do wonders in learning how to deal with your diagnosis and treatment options.