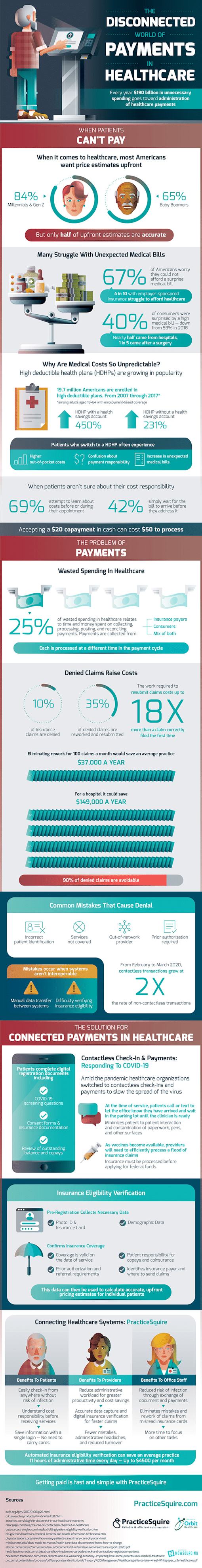
One year later after the start of the global pandemic, many are heading away from telehealth visits, and going back to in person doctor visits. There is no question that collecting payments on the payer side and going to the doctor during COVID-19 has become an increasingly complex and disconnected process.
Why is healthcare such a complicated process? Let’s explore some of the reasons below:
Many people struggle with unexpected medical bills. In fact, a shocking 67% of Americans worry they could not afford a surprise medical bill. Where do all of these unexpected medical bills come from in the first place? Over half come from hospital visits, and a full 1 in 5 come from a surgery. Much of the costs have to do with High Deductible Health Plans (HDHPs) and they are rising in popularity as of late. Patients don’t typically ask about costs prior to any visits and procedures and many just wait for all the bills to arrive before they address anything.
The Complex World of Administering Healthcare Payments
It’s hard to imagine, but every year, $190 billion in unnecessary spending goes toward the administration of healthcare payments. If you’re a doctors office, trying to get your $20 copay in might cost you $50 or more to process. This is an endemic failure in the healthcare space, as a full 25% of wasted spending in healthcare is spent on the process of collecting, processing, posting, and reconciling payments.
How to Solve the Payments Problem
Is there any hope to make the situation better? Yes! Doing it right the first time. Before going through all of these complicated and messy steps, what if there was a way to collect by connecting all healthcare systems – including insurance card image processing with eligibility.
PracticeSquire has a solution to fit the modern market needs of the marketplace:
- Patients can take solace in a safe environment by interacting with an easy kiosk check-in.
- Providers can reduce their administrative overhead and finally have a solution with accurate data capture, so claims get processed correctly, and the first time around.
- Office staff can reduce the risk of infection by having patients fill out their info, without the need to have duplicate work with re-entering their patient’s information.
This level of automated insurance eligibility verification can help the average physician practice recoup up to 11 hours of administrative time every day – this amounts to up to $4500 per month.
Take a look at the following visual deep dive for more information:







Reply